The Melanie Avalon Podcast Episode #74 - Benjamin Bikman, Ph.D.
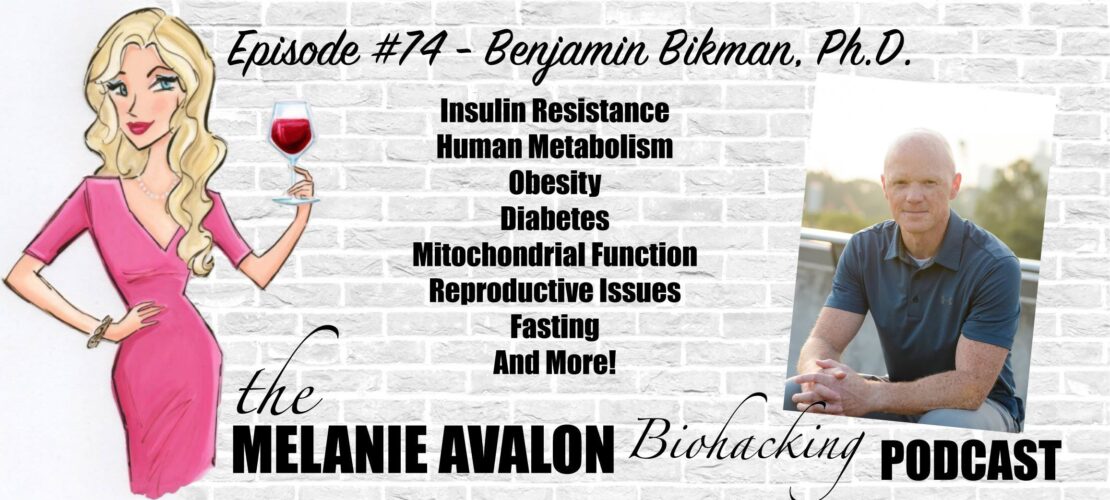
Benjamin Bikman earned his Ph.D. in Bioenergetics and was a postdoctoral fellow with the Duke-National University of Singapore in metabolic disorders. Currently, his professional focus as a scientist and associate professor (Brigham Young University) is to better understand the role of elevated insulin in regulating obesity and diabetes, including the relevance of ketones in mitochondrial function. He is the author of "Why We Get Sick", which explores a common factor that underpins most diseases.
LEARN MORE AT:
Twitter/IG: benbikmanphd
https://www.insuliniq.com/
getHLTH.com
SHOWNOTES
1:45 - IF Biohackers: Intermittent Fasting + Real Foods + Life: Join Melanie's Facebook Group For A Weekly Episode GIVEAWAY, And To Discuss And Learn About All Things Biohacking! All Conversations Welcome!
The Melanie Avalon Podcast Episode #70 - Kara Collier (Nutrisense)
Go To Melanieavalon.com/nutrisenseCGM And Use Coupon Code MelanieAvalon For 15% Off Select Packages
2:35 - Follow Melanie On Instagram To See The Latest Moments, Products, And #AllTheThings! @MelanieAvalon
2:45 - BEAUTYCOUNTER: Non-Toxic Beauty Products Tested For Heavy Metals, Which Support Skin Health And Look Amazing! Shop At Beautycounter.Com/MelanieAvalon For Something Magical! For Exclusive Offers And Discounts, And More On The Science Of Skincare, Get On Melanie's Private Beautycounter Email List At MelanieAvalon.Com/CleanBeauty! Find Your Perfect Beautycounter Products With Melanie's Quiz: Melanieavalon.Com/Beautycounterquiz
Why We Get Sick: The Hidden Epidemic at the Root of Most Chronic Disease―and How to Fight It (Benjamin Bikman, Ph.D.)
8:55 - Ben's Personal Story
13:15 - Insulin's Role In Disease
17:05 - Measuring Insulin
17:25 - What Is Insulin?
19:30 - Insulin Signaling
20:40 - Defining Insulin Resistance
21:35 - Insulin Resistance And Sex Hormones
23:35 - Fatty Acid Transportation
25:15 - High Blood Glucose; Low Insulin
25:35 - Gluconeogenesis
27:15 - Homeostasis Between Gluconeogenesis and Insulin
28:00 - Communication And Regulatory Signaling
31:05 - PCOS
33:05 - The Role Of Fat Cells In Insulin Resistance
34:30 - How We Gain Fat
36:55 - Insulin Resistance In Fat Cells
37:40 - Inflammation in Fat Cells
39:30 - Insulin Sensitivity In The Morbidly Obese
41:20 - The Role Of Hypertrophy Vs Hyperplastic Cells
43:35 - Differences In BMI Application
46:55 - Vitamin D, and K2
50:30 - LUMEN: The Lumen Breath Analyzer Tells Your Body If You're Burning Carbs Or Fat for energy! You Can Learn More In Melanie's Episodes With The Founder (The Melanie Avalon Podcast Episode #43 - Daniel Tal, The Melanie Avalon Podcast Episode #63 - Daniel Tal (Lumen)) And Get $25 Off A Lumen Device At MelanieAvalon.com/Lumen With The Code melanieavalon25
52:00 - Visceral Fat Vs Subcutaneous Fat
52:55 - Macrophages And Foam Cells
56:40 - Ceramides, "Bad" Fat In The Body
The Immunity Code: The New Paradigm for Immune Centric Health and Radical Anti-Aging (Joel Greene)
59:05 - Creating Insulin Resistance
59:40 - Inflammation And Ceramides
1:00:25 - Insulin Resistance In Muscle Vs Fat
1:03:40 - Glycogen Storage; Liver Vs Muscles
1:05:40 - Muscle Glycogen Usage
1:07:10 - Liver Glycogen Depletion and Ketosis
1:09:50 - Increased Glycogen Storage
1:12:10 - Water demands of glycogen
1:13:20 - Fat storage vs glucose storage
1:15:45 - Fruit Diets
1:17:40 - Non-essential Carbohydrates
1:19:30 - essential glucose
1:21:00 - carbohydrate conversion to fat
1:22:55 - Types of Fat Created by type of carbohydrate
1:24:20 - HFLC Vs LFHC
1:27:20 - How saturated Fat Impacts Insulin Resistance
1:29:10 - Saturated Fat in the Blood
1:30:30 - palmitate production
1:32:00 - Oleic acid storage
1:33:10 - Monounsaturated Fat's Protective Effect
1:34:00 - Natural Fats; Animal and Plant Saturated Fats
1:35:15 - Saturated Fat in a Mixed Macro Diet
1:37:10 - Order of Macro Consumption
1:41:05 - Carb + Protein Plant Sources
1:42:20 - SELF DECODE: get all of your nutritional questions answered with self decode's comprehensive genetic reports! Go To MelanieAvalon.com/getselfdecode For 10% Off With The Coupon Code melanieavalon and Don't miss a thing by signing up for Melanie's Private Email List At MelanieAvalon.Com/EmailList!
1:45:00 - Physiological Insulin Resistance
1:50:00 - Metabolic Inflexibility
1:54:00 - a practical diet including carbs
1:56:40 - Glycemic Load and Glycemic Index
1:58:10 - CGM Usage
1:58:40 - Berberine, Cinnamon, ACV for Glucose Control
Why We Get Sick: The Hidden Epidemic At The Root Of Most Chronic Disease―And How To Fight It (Benjamin Bikman, Ph.D.)
TRANSCRIPT
Melanie Avalon: Hi friends, welcome back to the show. I am so incredibly excited about the conversation that I'm about to have. For listeners who listen to my other podcast, the Intermittent Fasting podcast, I have been teasing this conversation in this episode for so long. Ever since I started listening to podcast interviews with this fabulous guest and then read his book when it came out, I knew I had to find him and have a conversation with him because he dives so, so deep into something that I think personally is so huge and not really discussed in the intensity and nuance that it should be, and that is the role of insulin in our health, in our diet, our fitness and all of the conditions that we're often experiencing today.
This wonderful guest, who I've been told I can call Ben, but I am here with Dr. Benjamin Bikman. He is the author of Why We Get Sick: The Hidden Epidemic at the Root of Most Chronic Disease, and How to Fight. Friends, get this book. Well, listen to this episode and then get this book. I have so many questions for you, Ben. Thank you so much for being here.
Dr. Benjamin Bikman: Oh, Melanie, my heavens, what a generous introduction. I am delighted to be here and to talk about insulin and how relevant it is. At the end of this, I bet all your listeners will feel they've just kind of gone through a masterclass of human metabolism. At least that's my goal.
Melanie Avalon: Yes, it's a great goal. Let's do it. For listeners, a lot of you might be familiar with Dr. Bikman already having read his book or listened to different interviews that he's done. For those who are not familiar, he earned his PhD and bioenergetics. He was a postdoctoral fellow with the Duke-National University of Singapore in metabolic disorders. He is currently a scientist and associate professor at Brigham Young University. Like we just said, he has a focus on understanding the role of elevated insulin in regulating obesity and diabetes. I really wanted to bring you on the show, so I sought you out myself through your college email. Then, I think, a few weeks later, either your agent or publicist or somebody was like, “Can you bring him on the show?” I was like, “Oh, he's already coming on.”
Dr. Benjamin Bikman: Yeah, that's great. He's actually a family friend, so it's nothing so formal. I'm not polished enough to have my own publicist.
Melanie Avalon: Oh, well, he's doing a good job, he is so. I thought that was so great. Oh, and actually, it was also funny, last quick story. He sent me a copy of your book to read and then, the next day, I got another copy of your book from-- because I've been wearing a continuous glucose monitor. One of the companies sent me your book, and I was like, “Your book just keeps showing up at my door.”
Dr. Benjamin Bikman: Now, you can regift.
Melanie Avalon: I know. I'm good for Christmas. In any case, to start things off, would you like to tell listeners a little bit about your personal story and what brought you to where you are today, especially with your focus on metabolic health disorders, insulin brought you to write this book, all of that stuff?
Dr. Benjamin Bikman: Yeah. Thanks again. What a fun opportunity. My interest really started because of my interest in athletics. Now, I was never overly talented as an athlete, but I was always involved in athletics and interested in how to improve. That meant, at the end of my undergraduate degree, having studied Exercise Science, I felt that there was more to learn. I had really just become increasingly curious. That got me on the path to get a master's degree in exercise physiology, but towards the end of that, I was actually becoming increasingly disinterested in the muscle, which is what had been my primary focus, what are the signals that make muscles bigger and better? My interest had shifted to fat cells, and I was increasingly interested in why it is that if someone is overweight, they have such a significantly increased risk of so many diseases, not just type 2 diabetes, but also heart disease and certain cancers and liver problems, and on and on.
Then, towards the end of my master's degree, I almost accidentally stumbled across a manuscript that had been published just a few years prior. This would have been in the late 90s, is when this manuscript had been published. What it found was that fat cells released hormones, pro-inflammatory hormones called cytokines. These cytokines would drive insulin resistance through the body, and that was so eye-opening to me because it not only revealed to me for the first time, again, first time I had seen it, although there had been other instance, evidence for this prior, but that fat cells were endocrine organs. Fat cells are actively producing and secreting molecules that will tell other cells in far parts of the body what to do, and that is how we define an endocrine organ.
It revealed to me the fat cells or endocrine organs, something like the adrenal glands, or the thyroid gland. Also, that the fat cell then has a mechanism to help explain the connection to type 2 diabetes, helping us understand, at the time, this new term that was being coined “Diabesity,” this phenomenon, where we see obesity and diabetes always occurring together, it was perhaps because of these fat cells that were getting too big. So, that began an interest for me, to shift my focus away from exercise and to start looking more directly at disease, like obesity and diabetes, which is what I was mostly interested in at the time, and to do so through the lens of the fat cell, and that's what I was able to focus on in my doctoral work and more in my postdoctoral work, where it was more specifically studying a condition called insulin resistance.
If we sort of zoom ahead in time, I've been a professor for 10 years now. My first teaching assignment that I was given at my university was to teach a class called pathophysiology. Patho just means sick. Physiology is just the body's systems. By the time, the student is taking this class, they've learned how the body works when it works well. Then they start to learn how it works when it's not working well. Actually, full disclosure, I felt very inadequate for that job. I had never taken back to this day. I have never taken pathophysiology as a class. To have been given that as an assignment was a bit sobering for me. I felt somewhat prepared or qualified because my research focus had been the two most common metabolic problems, at least, obesity and diabetes. I thought, “Well, I can just sort of play to those strengths.”
When I developed the diabetes lecture, for example, I made sure to emphasize that there's this condition called insulin resistance that is really foundational to type 2 diabetes, it is the fundamental cause of the disease. Then when I would start preparing the lecture on say Alzheimer's disease, I wondered whether there might be some role for insulin resistance. I didn't know of any at the time where I'd heard just pincer whispers have it. But I thought, “If I can find some relevance to insulin resistance in at least it gives me something that I can speak on with some high degree of authority and maintain the respect of these little 20-year-olds.” So, I did so, and I was surprised at the amount of evidence that suggested that insulin resistance is in fact somewhat fundamental to Alzheimer's disease.
I did the same process and continued to be amazed, although increasingly less amazed, as it continued to become relevant that I just found that insulin resistance was really foundational in either directly causing or significantly contributing to virtually every chronic disease, from Alzheimer's that I've mentioned, to various forms of heart disease and elevated blood pressure, even the things as seemingly bizarre as infertility, like erectile dysfunction in men or polycystic ovary syndrome in women. The more I looked, the more I found that insulin resistance was playing a part. I thought that I had realized some important truth in how we look at disease. I thought, “This is something that ought to be not only understood more,” namely insulin resistance, but also appreciated in a clinical setting.” That was largely the impetus for the book.
I had this vision, which admittedly, I think is a little silly, and probably will never be realized, but of a patient talking with a doctor and the doctor looking at the patient's a steadily climbing glucose and steadily climbing blood pressure. Before just giving an anti-diabetic drug and an anti-hypertensive drug, the physician would pause, and then wonder, to what degree might insulin resistance be causal cure to these disorders, and then actually test for insulin resistance. Then, if it's found that the patient has insulin resistance, well, then that becomes the point of attack. The physician rather than giving these two distinct drugs, realizes that these drugs would simply be addressing symptoms of one common problem, and that would be insulin resistance. Once we appreciate the role for insulin resistance, we can address it through lifestyle, which is absolutely, quantifiably, the best way to improve the problem.
That's the long journey over the last 25 years of me as a curious undergraduate really, and then getting to the point where I am now, running the metabolism and diabetes research labs at my university. Understanding insulin is essential to understanding metabolic health.
Melanie Avalon: Oh, my goodness, I am loving this conversation so much. I'm having to stop myself because I have so many rabbit hole tangent questions that I want to ask, but I know we should probably lay down some foundational groundwork first. Actually, I have a story for you that you'll probably like because you're talking about your vision with a doctor, or with doctors and their relationship with patients and testing for insulin. Like I said, I've been wearing a CGM now for about a little bit over a month. We can talk maybe about CGM later in the show, but it's been really eye-opening for me. My fasting blood sugars, it's good, but I want it to always be better. I was talking with my endocrinologist and said that I wanted to work on my fasting blood sugars. She was like, “Well, it might be more beneficial rather than testing blood sugar for us to test insulin.” I was like, “Oh, my goodness.” [laughs] This is such a good moment.
Dr. Benjamin Bikman: That is not common. Yeah.
Melanie Avalon: I know. I was like, “I have to tell you.” The changes are happening, I have hope that it will continue to go that way. We can talk about measuring insulin, too. Mine was 4.5, which made me happy because I thought that it might be higher. In your book, you said less than six was a good thing to aim for. Stepping back a little bit. Insulin, this is a very basic question. What is insulin? What makes it unique in the body? I love how you talk about how it really does affect? I mean, I don't know if it affects every cell.
Dr. Benjamin Bikman: Everyone. No, you're right, literally every cell. I don't use the word literally too liberally. Literally every cell.
Melanie Avalon: Wow. See, that's huge.
Dr. Benjamin Bikman: Oh, it matters. Insulin is a small little, what's called a peptide hormone. Basically means it's like a little protein that the pancreas makes, and everyone makes it unless the person is a type 1 diabetic. Type 1 diabetics have lost those insulin-producing cells, because insulin is essential for survival, then then the type 1 diabetic will survive and thrive by giving themselves daily injections of insulin. We need it, it is essential. Every cell, like we mentioned, every cell in the body will respond to insulin. There are insulin receptors on every cell. Basically, little doors that only insulin will come and knock on. When we typically look at insulin strictly through the lens of glucose control, but that's tremendously unfair. Insulin can elicit dozens, hundreds of different cellular processes in the body, in the cell, in every cell, but it's true insulin does control glucose, and that's certainly what it's mostly known for.
When someone eats a starchy or sugary meal, blood glucose levels will climb, that is unhealthy if they are elevated for too long. In fact, it's actually lethal. Thank heavens, we have a molecule that can come in and knock on the doors of cells. Then in certain cells, not all, in certain cells, that knock will result in different doors opening, allowing the glucose to come rushing from the blood into the cells for the cells to either use for energy or to store for later use. Whether it stays stored as glucose or whether it gets converted to fat, just depends on the cell. Insulin tells cells what to do with energy. That's really the theme of insulin because insulin doesn't stimulate glucose uptake into every cell. For example, it does tell the muscle cells to take in glucose, but it doesn't tell the liver cells to take in glucose. The liver can just take in glucose without insulin, but nevertheless, insulin will tell the liver what to do with the energy that it has in the theme, again, insulin theme is to store energy. Insulin wants cells to take in macronutrients and things like amino acids, and to make bigger molecules from them. Whether it is taking in glucose or fatty acids to make triglycerides to store fat, or whether it's taking in glucose to create glycogen, to store glucose, or whether it's stimulating the uptake of amino acids to make new proteins into those cells, and many, many more. Insulin is anabolic, it will stimulate a cell to store energy that's its theme.
Now, in the case of insulin resistance, which is the main point of my research in a way and the main point of the books most certainly, insulin resistance is when two things are happening together and they always happen together. That is when some cells, not all, but some cells have stopped responding to insulin pressure properly, and we have elevated insulin. That is such an important second or other side of the coin. It's not just a matter of insulin not working well and all cells, that's a part of it. That's why we define it as insulin resistance because, for example, the muscle cells, they do become insulin resistant, and that means they cannot take in as much glucose, because of muscle is the main consumer of glucose. If its glucose uptake is compromised, now we have glucose lingering in the blood, and thus we would see a person's blood glucose climbing over time and just genuinely be elevated. Other cells don't become insulin resistant. Now they suffer because the insulin is too high. Now insulin is over activating them.
One incredible example is a type of cell in ovaries. There's a type of cell in ovaries called the theca cells. Theca cells are the cell that's responsible for converting testosterone into estrogens because it's a little-known fact. All estrogens in men or women were once androgens, namely testosterone. It's just that the testes and the ovaries convert these androgens into estrogens. Of course, the ovaries do it more than the testes do, which is why women have higher estrogens than men do. The theca cells respond perfectly to insulin, they do not become insulin resistant, but because the insulin levels themselves are higher. Now insulin is doing too much at the theca cells. This too much actually is activating an enzyme that inhibits the conversion. It blocks the ovaries, the theca cells from converting androgens to estrogens, and so the women now has ovaries that are releasing too many androgens, making her body hair a little more coarse, making her facial hair more coarse, even making her go thin on her hair on top like typical male pattern baldness. Also importantly, she doesn't have enough estrogens being produced. That means the menstrual cycle is disrupted. Then she may have follicles developing in her ovaries, but never one that actually ovulates. All those little follicles stick around making the ovaries get several times bigger than they should as they're loaded with follicles. Thus, she has PCOS.
Insulin resistance, again, just so that we have a common kind of definition here, it's a problem where, first of all, some cells in the body aren't responding well to insulin. And then second, insulin levels themselves are higher than they were before. Those two together is what we should define as insulin resistance when we think of it in a person.
Melanie Avalon: Okay, this is so great. I have so many questions to that.
Dr. Benjamin Bikman: Yeah, that was a big dump right there, wasn't it? There was a lot of info.
Melanie Avalon: One quick clarifying question. So, you're talking about how insulin is responsible for ushering energy into cells or unlocking cells to accept energy. You talked about glucose and amino acids. Does insulin usher fatty acids into cells?
Dr. Benjamin Bikman: Yeah, that's a great question. Insulin is necessary at some basal level for there to be these fatty acid transporters, but if insulin goes up, it doesn't stimulate the fatty acid transporters to be any more active. Elevated insulin isn't necessary for fatty acid transport. It is most certainly necessary for glucose transport, and to other degrees, varying degrees, also essential for amino acid transport.
Melanie Avalon: If we're in a really low insulin state, fatty acids can still be going in and out of cells, but glucose would just be coming out. Well, I guess would be in a fasted state.
Dr. Benjamin Bikman: No, you're right. If insulin is down, a fatty acid could still go into a fat cell, any cell to be used. A muscle cell would greedily gobble up fat to be used for energy. In a fat cell, as fat would be coming in to be stored as triglyceride at this because insulin is low, you would actually be a net efflux or net loss of fat where you would be breaking down more fat than you would be taking in, but it would still be taking fatty acids in.
Melanie Avalon: I don't know if the situation ever happens, but I'm just trying to understand how things go down. If a person let's say they had high blood sugar from gluconeogenesis, from the liver, but they were like low insulin, like with that glucose in the bloodstream, not be able to enter any cells except for like muscle because of them stimulating?
Dr. Benjamin Bikman: What a great question. No, I love what you're thinking. So, you're really kind of weaving together some excellent interesting biochemistry here. Yes, so gluconeogenesis, as you note, is the process whereby the liver is making glucose from kind of scraps, and in fact, the predominant scrap is actually lactate. Lactate provides the backbone for almost for the majority, I think is about 60% of all the glucose that is produced from the liver, in gluconeogenesis, it might actually be more. Nevertheless, if insulin is down, gluconeogenesis will be activated and so to would glycogenolysis, the breakdown of glucose, of stored glucose in the liver. What wouldn't happen is, it would never produce so much glucose to result in a big insulin spike. What happens in that sort of-- it would be a fasted state is the most obvious instance of this.
If a person's fasting, insulin has come down, and that disinhibits these glucose producing processes in the liver, insulin basically gets out of the way. Now the liver starts releasing glucose, and that means the pancreas will still be producing insulin, because if there's glucose in the blood, then you need insulin in the blood, the beta cells of the pancreas would be stimulated to continue to release insulin, but it reaches this low basal agreement, where the liver is producing enough glucose, which is driving a certain amount of insulin production from the beta cells, but it's not too much insulin because of insulin went too high, then it would turn off those glucose producing processes in the liver. They just come to an agreement, this homeostasis, where there's always this kind of basal amount of glucose being released, and a basal amount of insulin, but one never really triggering the other. If glucose got too high from that gluconeogenesis, then it would stimulate a big insulin spike, and then the insulin spike would turn off the gluconeogenesis. Which if they're fasting wouldn't be good, because then you have some cells that would starve because of the lack of glucose.
There's this yin and yang, this delicate orchestra, where these two instruments gluconeogenesis and insulin start to play together, but quietly.
Melanie Avalon: That was one of my big questions, so I'm glad you went there. There's the bloodstream and the glucose in the blood, and we have the liver that can create glucose, we have the pancreas that can release insulin. Then, I'm assuming we have the brain, where's the monitoring happening? That communication between these different organs and the bloodstream? How are they communicating?
Dr. Benjamin Bikman: That's a great question. I would say that it's communicating directly. There's a direct communication between-- well, I shouldn't say direct, it really is the two signals of glucose and insulin, well, in others to be honest, during fasting glucagon becomes relevant as well. There are these inputs that are going to be signaling at the liver and the pancreas. From the pancreas, we would have signals like, let's just say insulin, I guess to keep it simple, that if it had its way, it would be telling the liver to stop releasing glucose. Insulin abhors breaking molecules down, that is catabolic, which is antithetical to insulin‘s anabolic role. If insulin had its way, it would be stopping any cell from sharing any energy, including the liver breaking down, glucose or making glucose, but also even the fat cell from releasing fats. And so, the insulin settles down to a basal level, like your fasting insulin of four micro units per mil, that would be a basal level, that would not be inhibiting. It would be tapping the brakes a little bit on the liver. It would also be tapping the brakes a little bit on ketogenesis. Insulin abhors the production of ketones. I say abhors as if insulin has a personality and a will of its own, but you know what I'm saying.
Melanie Avalon: I think it helps create a picture.
Dr. Benjamin Bikman: Okay, good. Insulin wants to inhibit the breakdown of glycogen and the production of glucose. It also wants to inhibit the breakdown of fat and the production of ketones. Say the four micro units per mil that you have, it's not enough to inhibit it all the way. It's just tapping the brakes a little bit. That basal level of insulin is partly driven by the basal amount of glucose that the liver itself is releasing. There's no one single point of regulation. It's going to be a mix of regulatory signals at the pancreas, at the liver, constantly relying on the signal coming from the other. The pancreas is constantly relying on the glucose, which is the signal coming from the liver, if you will, and the liver is constantly relying on the signal from the pancreas. For example, insulin, but also glucagon knows what it should be doing. They're each relying on the signal from the other to make sure that they're playing harmoniously, or in other words, maintaining homeostasis. The ketone, of course, that's-- I didn't necessarily mean to bring in that topic now, but it's just more reflective of the overall role that insulin plays, in truly being the master regulator of fuel use in the body. I mean that, it has a role, it influences nutrient regulation in a way that, to my knowledge, no other hormone even comes close.
Melanie Avalon: This is so fascinating. You're speaking about PCOS. Is it accepted in the medical community that insulin is the cause of PCOS?
Dr. Benjamin Bikman: No, it's not. It's certainly very appreciated, but I know on social media, I've been somewhat grilled in the past, because people will invoke these instances of, “Well, what about lean women who have PCOS, and they obviously don't have insulin resistance?” I actually say, “Well, yeah, they probably still do actually.” I very much defend that perspective, because I'm a scientist and I try to be a good one. That does mean that I also need to be humble. What I mean by that is, I certainly suggest that insulin resistance is absolutely essential to polycystic ovary syndrome. I also would humbly acknowledge, there could be an instance where insulin resistance isn't the fundamental cause, but I don't know of it. Even in the case of the lean woman who then say, “Well, she's lean and she's not overweight and diabetic.” There was a study published just a few years ago that found that even in lean women with polycystic ovarian syndrome, with ovary syndrome I mean, they still have insulin resistance in their fat cells that you can detect a significant amount of insulin resistance in their fat cells, even compared to other women of comparable body size, who don't have polycystic ovary syndrome.
Even when you look in the lean woman with PCOS, it's almost certainly the case that she still does have insulin resistance, it just isn't going to be quite as whole-body or universally obvious throughout her body. When you do some tests to look at the insulin resistance in the fat cells, which I think is relevant, because I actually believe that's where insulin resistance starts, then you detect the insulin resistance, nevertheless. Even though she doesn't fit the profile, if you will.
Melanie Avalon: Yeah, that's one of my current obsessions, and you touched on it multiple times already in this conversation. That's the role of fat cells and insulin resistance. I think I first started getting really interested in this when I was at a very low weight and wanting to gain weight. I was researching, how fat cells gain weight. I was learning how a lot of people who are actually thinner, underweight may actually have fat cells that are potentially more inflammatory or more insulin resistant. In your book, you talk all about the difference between fat cells that split and form new fat cells versus fat cells that just grow and become inflamed and inflammatory. Would you like to talk a little bit about this? I just find this so fascinating.
Dr. Benjamin Bikman: When insulin is elevated, and there are sufficient calories available, and that doesn't mean the person has to be necessarily in so-called excess of calories. I'm a little cool when it comes to speaking about how important calories are. I think they matter, but they're given too much attention. I think part of that attention needs to be divided between calories and insulin. An insulin is elevated, it will signal fat cells to store energy. This would be someone who's gaining fat mass. Now a body can gain fat mass through two mechanisms. One being much more common than the other, and that would be the first one that I'll mention.
When insulin is elevated and there are sufficient calories that the body is storing fat, most commonly, you will store fat through what's called hypertrophic fat cell growth. That's where, like you said, that's when the person's number of fat cells is set, it doesn't change. As the insulin is telling it to store more energy as fat, that means each individual fat cell must carry a greater burden. So, the individual fat cells begin to grow. That is hypertrophy. We have hypertrophic fat growth. Again, that is the most common. Most people once they finished puberty, late teens for girls and early 20s for boys, they will have a set number of fat cells, they're done.
Now fat cells can die. They have a lifespan of about 10 years, and they can be replaced. Generally, the number of fat cells is essentially fixed. Of course, nothing is ever truly fixed in the human body. It's constantly dynamic, but generally they're done. They're not going to expand their fat cell number. That is why most people if their insulin is elevated over time, in their sufficient calories, they will get fat through hypertrophic fat growth. Then in contrast, or alternatively, some people genetically, and partly through perhaps foods they eat. There could be a dietary component to this, they will get fat through a mechanism called hyperplasia or hyperplastic fat growth. That is when they maintain the ability to make new fat cells all the time. This would be a fat cell, or fat cells that start to get a little big because insulin is stimulating their growth because they're sufficient calories. Then right before they get too big, they will recruit new fat cells. They have new fat cells that move into the neighborhood and they can start sharing some of this energetic burden. Basically, it's like the hyperplastic fat cells always have more room. They always have vacancy. Whereas the hypertrophic fat cells are full. There's no vacancy, they cannot handle any more fat to store.
Now, what starts to happen, then over time, is that the hypertrophic fat cells reach a maximum dimension, they're essentially as big as they can get. And yet, if insulin continues to be elevated, there's no choice but the fat cell to-- they continue to get that signal to grow. But, of course, it cannot grow anymore. The fat cell out of really self-survival, self-interest, starts to downgrade its sensitivity to insulin, it's basically saying, “Insulin, you want me to continue to grow, I cannot, I'm as big as I can get. So, I'm not listening to you anymore.” Now that fat cell starts leaking fat, it starts breaking down fat when it shouldn't. It shouldn't be breaking down fat. It still can take fat in, because insulin doesn't really drive that process anyway. So, fat can still come in, but now insulin can't stop it from breaking fat down. So, you have a fat cell, it stays big, unfortunately, it does not start to shrink, but it starts to break down its fat. That's why you have this big increase in free fatty acids, because the fat cell is no longer listening to insulin in that regard.
Also, at the same time, you mentioned inflammation, as these fat cells are getting so big, they run the risk of getting too far from capillaries, from blood flow. Every cell, of course, must have access to blood to survive. They need the blood to exchange gases, like carbon dioxide and oxygen, as well as to just exchange like metabolites and other molecules. As the fat cells are getting so big, they're getting too far from capillaries, and this may be part of the reason, they will release pro-inflammatory proteins, some of which help to stimulate the growth of new blood vessels. These two situations, these two products of the hypertrophic fat cell, namely, the leaking of the free fatty acids, and the pro-inflammatory cytokines are the fat cells effort to survive. Every cell is determined to survive, even in the midst of this onslaught of insulin and energy. In the process, unfortunately, releasing the free fatty acids and the pro-inflammatory cytokines, that's likely the mechanism whereby the hypertrophic fat cell starts spreading its insulin resistance through the body, to the brain, to the muscles, the liver, the pancreas, and the blood vessels, and so on.
Now, in contrast, again, the hyperplastic fat cells, they can continue to store more fat, and so they can continue to respond to insulin, because they don't ever since the crisis, that the hypertrophic fat cells, the individual cells are small, they can continue to store more energy. Once they start to get far from blood, or too big, they just recruit new fat cells. They maintain insulin sensitivity. Interestingly hyperplastic fat growth, it creates this paradoxical situation where the person can become morbidly obese. These are the kinds of people that are four or 500 pounds, where the average person simply could never get that big, the average person cannot get that fat, but these are people who can, and they maintain a high degree of insulin sensitivity, paradoxically, and that's what I meant by paradox, where they are morbidly obese have a fantastic amount of fat tissue, and yet they maintain insulin sensitivity. They may not be healthy in other ways, but their glucose will probably be normal, their blood pressure could be close to normal. Then, in the end, they're surprisingly healthy, healthier than you think.
In contrast, the average person who's growing their fat through hypertrophic fat, they reach a limit, their body, is that point where the fat cells become insulin resistant. Typically, at that point, they won't get fatter. Well, although they may start to store their fat ectopically. Now they start storing more fat in their liver, or even more in their muscle. I mean, the body of insulin is elevated, the body is determined to store energy. At that point, they generally reach a level beyond which they won't gain weight. So that's the differences between hypertrophic and hyperplastic fat growth and even some insight into why the hypertrophic fat cells become insulin resistant. Of course, a why question is the philosophy of physiology, and maybe someone would say, “Well, that has no place in hard sciences.” I like to joke with my students that when we ask a why question like, “Why do the hypertrophic fat cells become insulin resistant?” I presented the idea that it's their efforts to survive. I don't really know that. I joked that that's a divine question. God only knows why the cell acts the way it does. We don't know why the system was designed that way. We can only speculate. That's my speculation.
Melanie Avalon: Well, actually, my question I had is a why question.
Dr. Benjamin Bikman: I love them.
Melanie Avalon: Okay, good. Do you have any thoughts about why evolutionarily, like some people would have a tendency towards hypertrophy and others towards the hyperplastic? Is there a situation where there's a benefit to one versus the other?
Dr. Benjamin Bikman: Yeah, I do. This is, again, a matter of speculation, which is fun. Frankly, I could imagine that part of the difference would be where people's ancestors lived. Namely, cold climates or warm climates. In a cold climate, there is some survival with regards to being able to store fat, especially in the subcutaneous space, or the space under the skin, in order to preserve body heat, it becomes a form of insulation. In contrast, if someone is living on the equator, for millennia, theoretically or longer, theoretically, that is a person who would have no need of insulation, and perhaps, would have a limited capacity for fat growth. I say this is all much, much speculation, of course, but we know that there are certain ethnicities who suffer from fat mass sooner than other ethnicities.
For example, I did my postdoctoral fellowship in Singapore of all places, because of that government's high interest in some of the ethnic disparity with regards to diabetes. For example, if you take someone of, let's say, Malaysian ethnicity, which is the native ethnicity to that part of the world to the Southeast Asia. If you take that kind of almost a version of like Pacific Islander, which actually, I also could use here, it just wasn't as relevant, of course to Singapore. Take someone of say, like a Pacific Island, Equatorial descent, and compare them to someone who has, say, Northern European descent, like some of my ancestors, my kind of scotch Irish mix of Scandinavian, very North climate, very used to a northern climate, very cold, of course, at certain times of the year. Not only would they have needed more fat during the winter for warmth, but also more fat to survive on during the winter when food was scarce, as opposed to an equatorial ethnicity, if you will, if I can say that, where food is always abundant, and the temperature is never cold. There's simply not a real reason to store more fat. We start to see some of this play out, where at very much--
If you take a Northern European ethnicity and compare that with, say, a Pacific Islander, or Southeast Asian ethnicity, and they start gaining fat at the same rate, the Pacific Islander or Southeast Asian ethnicity will start to suffer from that much, much sooner than the Northern European. So, they will be moderately overweight. Now, say the Southeast Asian will now start to have elevated glucose, they will have hypertension, they're going to be on some medications for those and more. Whereas the Northern European, they're moderately overweight, and they're perfectly fine. They don't have any deficits, so to speak with regards to their health. That might be part of the reason why some people, why different ethnicities are more inclined to disease.
In fact, this is sufficiently real that there is a different set of BMI scales that are used for different ethnicities. For example, Southeast Asian ethnicities have a bit more of a rigorous scale with-- say Caucasian ethnicity, overweight doesn't start until 25. Obesity doesn't start until a BMI of 30. BMI is just of course you know and your listeners, I'm sure too, just a function of height and weight, so it's not great. With Southeast Asian ethnicities, and Asian ethnicities in general, it's shifted down like five points were overweight is like 20. And obese is considered 25, or something like that. I'm sure I'm not exactly right. But it's a different scale to more accurately reflect the risk of excess body weight across distinct ethnicities.
Melanie Avalon: Oh, I did not know that. With the BMI scale, I don't know how major populations [unintelligible [00:39:43] it, but really Arctic populations, would the BMI scale be-- probably should be higher, the numbers higher?
Dr. Benjamin Bikman: Yeah, that's right. Now, it doesn't play out quite like I described. For example, I think African ethnicity actually follows more closely to that Northern European. I probably ought to be more familiar with this. I think someone is listening to this could probably very likely start poking holes in some of what I described. I would want to be clear, I'm speculating on some of this, but it's a why question. There's a lot of philosophy involved or wondering. That's some of my wondering. I suspect it has something to do with climate and seasonal access to food or not. It's interesting also to note the differences, of course, in pigment, where the Northern European in getting relatively little sunlight because of such a fair, pinkish pigment is able to make a lot of vitamin D very quickly. As opposed to someone who evolved at the equator, who's exposed to sunlight all the time, it was a survival mechanism to have a darker pigment, and thus survive in that constant sunlight, but also now need more vitamin D. In effect, not to change the topic, I believe that's necessary to appreciate for us to appreciate the viral concerns taking over the world at the moment, and the ethnic disparities there. There's something incredibly relevant about vitamin D. To acknowledge the role for vitamin D and optimal immune health, we really need to scrutinize or appreciate the role of ethnicity as well.
Melanie Avalon: Speaking to that, what do you think about the differences between vitamin D from the sun and then based on your skin type, compared to the natural form that might be in things like fish, compared to like supplemental vitamin D? Do you have thoughts on that?
Dr. Benjamin Bikman: Yeah, a little. I'm certainly not a vitamin D expert. Of course, I'm a huge fan of natural vitamin D, including that which we make from exposure to the sun, which is based on cholesterol, and other reason that cholesterol is an absolutely essential molecule for animal life. In the sun, we will make vitamin D from cholesterol. Then alternatively, we can eat it in foods from animal source foods. I'm extremely favorable. I'm not favorable with regards to most supplements, but vitamin D3 is one that I'm absolutely an advocate of. I do think people should take vitamin D3 and, and K2 supplements, those two work well together now more than ever, with regards to COVID. Especially a clinical study, which confirmed that vitamin D therapy is extremely useful to COVID immunity.
Melanie Avalon: I've been supplementing with vitamin D for quite a while. I used to live in California, so I was always better with my vitamin D levels there. Now, I'm in Atlanta, and I've been able to raise my vitamin D blood with supplements pretty well. Then I also will do small tanning bed exposure during the winter, for like a minute to the UVB-only rays.
Dr. Benjamin Bikman: Yeah. Given your fair complexion, you can do that, you can get away. You're are able to make a lot of vitamin D very quickly. I think that really matters where people are talking about how COVID appears to really have a greater relevance in people of color, and I do think that's partly a result of our isolated existence nowadays, where we just aren't-- especially nowadays, if we're on lockdown, you can't go outside. The little bit of sunlight that you can get, if you're very fair complected, well, then that might be enough for you to get adequate vitamin D. If you have a darker complexion, then you need more time in the sun to do that. It's an advantage to have a darker complexion, of course, if you're in the sun all the time. I mean, for me, I will sunburn painfully depending on the day, like within 10 minutes, I'm so fair, it's such a curse. The flip side is, I'm in the sun for one minute and I got my dose of vitamin D for the day. I do think that it's part of the reason we do see some disparity across ethnicities with how vicious COVID-19 can be, all the more reason, in my mind, well, one to get outside as much as possible, but also to focus on vitamin D3 in particular.
Again, I'm pretty lukewarm on most supplements but that is one I very much advocate. Anyone listening to this, if they have a darker complexion, then all the more reason really get some vitamin D3, and I would recommend that it be coupled with K2. Get it today and start taking it, and you'll do yourself a favor.
Melanie Avalon: Going back to-- because I want to touch on one more thing that you were talking about with the fat cells, and talking about fat storage in visceral fat versus subcutaneous fat. Is the visceral fat more likely to be that hypertrophy type? The reason I asked that is because you talked about a study in the book when they took obese mice and took their visceral fat and gave it to lean mice, the mice became insulin resistant. When they took the subcutaneous fat from obese mice and put it in lean mice, they did not become insulin resistant. Is it because the fat in visceral fat just has more-- talking about it as like an endocrine system has more inflammatory markers, or why is visceral fat, so bad?
Dr. Benjamin Bikman: Yeah. Visceral fat appears to become more occupied by immune cells, like macrophages than subcutaneous than it does. Now that in and of itself is not inherently bad. Macrophages are everywhere. We have macrophages in the brain, in the liver, in the muscles, in the bones. We call them different things in different cells, partly because it wasn't until later that we realized that it was in fact all the same macrophage, we didn't know. We called them osteoclasts in the bone, and we call them Kupffer cells in the liver, not realizing at the time that, “Oh, wait, they're just all macrophages.”
Melanie Avalon: Osteoclasts are macrophages?
Dr. Benjamin Bikman: Yeah. Isn't that interesting?
Melanie Avalon: Really?
Dr. Benjamin Bikman: Yeah.
Melanie Avalon: I didn’t know that.
Dr. Benjamin Bikman: Yeah. They're everywhere, and we just call them different things, because they have slightly different actions depending on where they are. A theme of them is immunity and inflammation, and that’s not a bad process itself. Of course, inflammation is essential to healing and recovery, but it's just when we have too much of it. In the case of the visceral adipose, it becomes more occupied by macrophages more readily than subcutaneous fat does. That might be once again, on purpose, where perhaps the visceral fat, if it starts to get too big, you could see the problem where it would start to physically compress tissues, it would physically compress the intestines, it would physically compress the kidneys, blocking blood flow, so that the body very much has an interest in keeping visceral adipose in check. And perhaps the macrophages are there to help clear out some of that fat, and they would do so perfectly well, in a case of a modest amount of visceral fat if they needed to be there at all.
The problem is, if the person is continuing to develop subcutaneous fat, the macrophages themselves start to become loaded with that fat, and they become what's called foam cells. We call them foam cells, because if you actually look at them under a microscope, they look like they have a bunch of little bubbles. Yeah, they look bubbly, but it's actually just little pools of lipid or pools of fat. These foam cells are very pro-inflammatory, releasing a broad spectrum of pro-inflammatory cytokines thereby causing inflammation in the body. Inflammation is one of the fundamental causes of insulin resistance.
Melanie Avalon: For listeners, just to paint a better picture, the visceral fat is-- like we said, it's the fat around internal around the organs. The subcutaneous is what you can pinch, it's like under your skin.
Dr. Benjamin Bikman: You have to pinch in the jiggle, which is good. I would actually say all fat is good. I'm a great defender of fat, frankly. If I ever write another book, I don't know that I will, the first one was so exhausting, but if I ever write another one, it will be about fat. Just help people understand it, but you have a subcutaneous fat especially, it plays an essential role in human function, even including fertility. The reason, a little girl, for example, or a woman if she becomes infertile, or stops ovulating because she gets too thin, it's because the lack of fat, and it's fat hormones that actually allow the brain to drive fertility. Woman is more susceptible to this than the man simply because the woman really bears the metabolic burden of childbirth. She of course grows the baby and then feeds the baby, so she bears the metabolic burden.
A man can get phenomenally lean and maintain fertility. Of course, as a woman gets increasingly lean, then her fertility starts to become at risk because she needs more of a signal from her fat in order to allow her brain to promote fertility. That signal is leptin, and that's my point. Subcutaneous fat makes more leptin than visceral fat does.
Melanie Avalon: Okay, gotcha. Also, to that point, because you talk about in the book, ceramides.
Dr. Benjamin Bikman: Ceramides, yeah.
Melanie Avalon: I actually just recently had Joel Greene. Do you know Joel Greene?
Dr. Benjamin Bikman: I don't, it sounds familiar.
Melanie Avalon: He wrote a book called The Immunity Code. It's all about the role of macrophages and inflammation and body weight and stuff like that. He talks a lot about like 4-HNE, for example. That was the first time I was reading about that. Then I was excited to read in your book. What is it? Ceramides? Ceramides and what determines when fat becomes bad fat?
Dr. Benjamin Bikman: Yeah, that's right. What flips the switch from good to bad. In this case, yes. Ceramides are part of what likely-- not likely, definitely, ceramides make a cell insulin resistant. Now I say, I was hedging that a little bit, just because I wouldn't want someone to think I'm suggesting it's the only signal that can make a cell insulin resistant. No. I'm not saying that, but for a fact it does. I know that for absolute certain having done these experiments myself. Ceramides are a type of fat. When I say type of fat, it's because a cell will have-- they're literally like 1000s. 1000s of different types of fat within every single cell in the body. Ceramides itself is one class of an enormous class of fats, which itself encompasses another 1000s of types of fats.
Some of these ceramides, which are made in a cell, as a result of inflammation-- actually let me back up, they're essential. A cell has ceramides because you need ceramides for survival. If you have, say, an animal model, an animal like a rodent, a genetically modified mouse, and you have blocked those little embryos in mama mouse from making ceramides, those babies will be born but they will die. Blocking ceramides is incompatible with survival, you have to have them. As happens so often in the body and the intricacies of cell biology, you must have something, but you must have it at the proper levels. Insulins no exception. You need insulin, but you don't want too much. You need ceramides, but once again, you don't want too much. So, if a cell is accumulating ceramides, ceramides becomes-- it begins to directly antagonize what insulin is trying to do.
An insulin binds on a cell, it will initiate a series of events. A biochemical cascade or a chemical pathway. There'll be a series of proteins that basically start acting on each other in a sequence. Ceramides will get in the way of that. It will stop some of these proteins in the cell from passing this signal along basically, in this game of telegraph. Ceramides gets in the way of that and stops the signal, thus preventing the cell from responding to insulin as it would normally. That is the process whereby ceramides will cause insulin resistance, is basically a direct interruption of the insulin signal.
Melanie Avalon: Are they-- the fat cell protecting itself in a way?
Dr. Benjamin Bikman: Yes, that's a good question. Thanks. Ceramides will be made as a result of inflammation, like some of those same inflammatory signals we spoke about earlier, those cytokines, they will stimulate the synthesis of ceramides. Also, chronically elevated insulin will stimulate ceramide production. But, yes, if ceramides are accumulating in a fat cell, they will block the fat cell from being able to create new fat cells and force the fat cell to grow through hypertrophy. You'd mentioned for 4-HNE, which is a metabolite of linoleic acid, the Omega-6 polyunsaturated fatty acid, that also plays into this same process at the fat cell, preventing hyperplasia and forcing strict hypertrophy.
Melanie Avalon: Here's a question I had, because you talk in the book about how fat cells become insulin resistant first, muscle is also one of the first things to become insulin resistant. Why in the case of insulin resistance to fat cells--? I mean, I know there might not be “listening to insulin,” but we get fatter with insulin resistance, but with muscles, we lose the muscle. It's like the opposite.
Dr. Benjamin Bikman: Yeah. Right. The muscle, it doesn't respond to insulin, of course, the same way that fat cells do, being a very different cell, very different purpose in the body. Insulin protect muscle protein. It's not it doesn't appear to be essential in-- Well, a basal amount of insulin would certainly be essential for the muscle to make any protein at all. But spiking your insulin doesn't really appear to be necessary in facilitating muscle growth. I think sometimes people overexaggerate insulin’s role as an anabolic hormone at the muscle. It doesn't appear to stimulate any greater muscle growth when it's elevated, but what it does do is protect the muscle protein. It's anti-catabolic, as much as we could say it's anabolic, it's anti-catabolic. As the muscle becomes insulin resistant, insulin’s ability to defend a muscle protein becomes compromised. And now the muscle, the proteolytic processes, the catabolic processes start to dominate, as insulin’s losing that tug of war. The catabolic starts to win over the anabolic signals because insulin simply can't do it anymore.
Now, there are other anabolic signals at the muscle, just for full disclosure, like growth hormone, for example. Insulin is one of those signals that helps the muscle defend its protein. As the muscle becomes insulin resistant, then it loses that defender. Of course, the muscle never, not of course, someone wouldn't necessarily know this, it never becomes growth hormone resistant. There are other signals that are still trying to defend the muscle, the loss of insulin is pretty fundamental. That's why with insulin resistance, a person can start to develop sarcopenia or muscle wasting. Unfortunately, that starts to feed on itself, in a way, compounding the problem, because if you start losing muscle mass, you start losing the main consumer of glucose, after a meal, muscle consumes up to 80% of glucose. As the muscles become insulin resistant, it can lose that effect by half. Now you have all this excess glucose that couldn't go into the muscle and has no place to go, and now it stays in the blood, keeping glucose high, but also in the process keeping insulin high. As insulin stays high, it continues to actually elicit or cause insulin resistance. One of the other causes of insulin resistance, I'd mentioned inflammation a moment ago, is chronically elevated insulin. Too much insulin causes cells to become resistant to the insulin.
Melanie Avalon: You said 80% of the glucose after a meal into muscles.
Dr. Benjamin Bikman: Yep, that's right.
Melanie Avalon: This is a huge question I've had for so long. I'm trying to get an understanding of this. Glucose and glycogen, and muscles and the liver, and the potential storage and usage capacity of muscles versus the liver. Let's say that there is room in our muscles and our liver. Does the liver always fill first and then the muscles, does it not matter?
Dr. Benjamin Bikman: That's a great question. Yes, so in the context of stored glucose, and that's of course called glycogen, which you said. Muscles are very greedy, and the liver is very giving. The muscle can store depending on the person, of course, and their amount of muscle. A normal-sized individual will store around 1200 to 1400 or so calories as glycogen in muscle. Then there will be anywhere from like 400 to 600 or so calories, is stored as glycogen in the liver. The muscle will store more, and that's just because there's so much more muscle. Several times order of magnitude probably more muscle than we do liver on an average-sized person. It stands to reason that the muscles have a greater overall capacity. The muscles, like I said, are very greedy, though. That has two effects. One, it means that the muscle never shares its glycogen with the rest of the body. It will only use it itself. If a muscle has stored glycogen, it is staying in that muscle. When the muscle breaks down that glycogen, it is simply to make fuel for that individual muscle cell, it will never release it into the bloodstream.
In contrast, the liver glycogen is meant to be actually shared with the body to give energy to other cells in the body, like the brain or the muscle. The liver doesn't use its own glycogen, it gives it up. So that's what I meant earlier there with regards to the liver being more giving, but that also reflects in the rate at which the tissue will replenish those glycogen depots and how reluctant the glycogen depots are to run out. If you and I were to start fasting now for 24 hours, we would run out of liver glycogen, because the liver will have given it all up by then. Our muscle glycogen would actually be probably normal. The muscle will use it very sparingly. Even if we wouldn't exercise, it will fill itself back up on glucose coming from the liver. The liver, the muscle will fill back up with glycogen much, much faster. In fact, it's virtually impossible, except with extreme exercise to run out of muscle glycogen. You can, however, very readily run out of liver glycogen just with a 12-16 hour fast and you'll be out.
In fact, that's the point at which the body also starts making more ketones, and the person becomes-- they get into ketosis, that is elegantly matched, where right around the time the liver’s running out of glycogen, the liver is also started producing glucose. That's the way of the liver as it runs out of one nutrient to provide the other for the brain. Of course, during fasting, the brain will shift to using 75%, 80% all of its energy from ketones. It's actually to, in a way, a reflection of the fact that the liver’s run out of glucose, and the liver saying, “Look, I'm running out of this, and so I'll give you something else,” the ultimate giving organ. That's why in the book, I actually joke about this. In Persian cultures, a term of endearment is to call someone your golden liver. If I were talking to my wife, I wouldn't say my sweetheart, the heart is actually, it's muscle. It's very selfish. I would say my golden liver, that's a term of endearment. I think there's something a little more beautiful about that because the liver is really so generous with regards to how it interacts with the body.
Melanie Avalon: I'm dying to know your thoughts on, do you think liver glycogen depletion is necessary to enter the ketogenic state or to start ketosis. Some people say that ketosis is not dependent on liver glycogen stores.
Dr. Benjamin Bikman: That's a good question. I think anyone saying this is speculating, because I've never seen a study that can confirm one way or the other. In fact--
Melanie Avalon: I saw one recently, actually.
Dr. Benjamin Bikman: They confirmed?
Melanie Avalon: It was in rats. I can send it to you, but I found it. It was like you're talking about getting when you find this study, and you're like, or you're reading it, you feel you're in a little dark cave reading this magical study.
Dr. Benjamin Bikman: Yeah, that's awesome. I don't believe is necessary for the record because ketogenesis is not a function of glycogen. It is a function of insulin, frankly. Those are very related, so it's in a way, I would say, well, we're sort of splitting hairs. I think the closest I'd found, although I'd love to see that animal study was the guy who did a lot of starvation work, George Cahill is his name, there was just some speculation in a way that these-- I would say this is definitely not causal. The liver running out of glycogen definitely does not cause the increased ketogenesis. It's probably coincidental.
Melanie Avalon: This is fascinating. That's huge what you're saying about ketosis not being dependent on glycogen, but it's about insulin. The study of the rats, it was looking at time to ketosis, and rats fed different diets and the liver glycogen, like how that related to the entry. The rats on the low-carb diet, it was a while since I've read it, so I have to look at it again. The rats on the low-carb diets-- I don't think their glycogen really affected when they entered. Their glycogen didn't really change that much based on different levels of ketosis. It was fascinating.
Dr. Benjamin Bikman: Rodents, they're so tricky when it comes to ketosis. We're actually battling some of that right now, we're doing a brain ketone study. It's so tricky to anticipate the rate at which the animals are getting into ketosis and how you have to manipulate the diet in such bizarre ways. It's so different from humans. Nevertheless, there's value in that finding and I'm glad to hear it. I would again, just say glycogen isn't going to be causal, or necessary for ketogenesis.
Melanie Avalon: One more liver glycogen question, this is one of my obsessions. What do you think about liver glycogen storage potential? Are you familiar with the people in the Ray Peat world?
Dr. Benjamin Bikman: No, not at all.
Melanie Avalon: He's a-- What is he? He has letters after his name, but he has done a lot of research. There's a whole community, but his whole tenants are-- He's very much a fan of actually like glycogen, fuel body, rather than fueling primarily on fatty acids. He talks about the stress response and thyroid and all this stuff. On PUFA depletion, it's one of his big things. A lot of people are talking about building up your glycogen storage potential. This actually ties into a question we can maybe get to, which is physiological insulin resistance versus glucose intolerance versus low carb, but do you think there is a benefit? If you're running on carbs, more as your preferred source of “fuel,” do you get better at processing them? Do you get better glycogen stores? You get better flexibility with that, compared to if you're in like a low-carb state? Do you lose your glycogen storage potential? Then I have a follow-up question, like I said about physiological insulin resistance.
Dr. Benjamin Bikman: Yeah, that is interesting. I would say if you have more mitochondria, and your training, I guess with-- I don't know what the training regimen would have to be, but you're training in such a way to rely more on oxidative glycolysis, which can produce more energy than anaerobic glycolysis, then you could be more effective or more efficient with your use of glucose. In other words, getting more bang for your buck. So, there's probably a way you can exercise to help train that and that might yield some improved glucose use. However, the idea of pushing the body to store significantly more glycogen than it would normally store, I would say that is-- I mean, we know that you can glycogen load, but if you take all the glucose and the average person's body, it's enough for about 2000 calories. Let's say you can expand your glycogen storage significantly and I know you can a little with training, but let's just say ridiculously you got another 1000 calories, in fact, that would have to be impossible, because the water weight that would come with that you would gain, you'd be so much heavier, because glycogen-- that's the problem with glycogen.
It is a very heavy molecule because of its water demand. Mind you, I am speculating, I bet it's impossible to even gain 50% more glycogen because your body mass would climb so significantly, like probably 20 or 30 pounds. I'm just throwing these numbers up on the wall at the moment. Glycogen is a very heavy molecule, because of the water load that comes with it. I would say there, there's a very limited degree of expanding your glycogen, not that it can't happen, it absolutely can. But if you are training in a way to use energy, and to not have to-- if your philosophy is, “I'm going to more efficiently use glucose and store more glucose, then you're going about it the wrong way because if you are trying to use an energy source more efficiently, and not only use it more-- I mean, fat burning, for example, I'll get to my point yields significantly more energy than any form of glucose burning by a lot. Fat storage is significantly more efficient than glucose storage.
Now, that's a problem in some people, of course, they're efficiently storing energy, that means they're gaining weight so easily, gaining fat. Even in the context of athletics, most certainly in the context of endurance exercise, if you can improve your ability to burn fat at ever higher intensities, this fat adaptation, I would say that's the ideal strategy. Truly, I mean, this with all due respect to that, that scientist, and I do mean that, I really suspect this person has put a lot of time and thought into that. I'm hoping that there's a common ground here that where I might be misunderstanding the purpose, but if the purpose is to efficiently use energy, and store energy efficiently, well, then fat does that already. Then you're simply focusing on the wrong macronutrient. All the more reason to become fat-adapted, because you can store orders of magnitude 10, or more often 100 times more energy as fat. Even the lean individual has plenty of fat stored, no need to try to glycogen load and go through all that discomfort, which is uncomfortable, and only to run out of the energy anyway, partway through a marathon where you have to then be including more glucose, you have to start taking more in, you don't have enough stored if you're relying predominantly on glucose. If in contrast, you've trained your body to rely at high intensities on fat, you don't need to take in any fat, you have plenty to go, so that you can avoid some of that GI discomfort that comes from having to ingest glucose in the midst of an event. You don't have to ingest any you just drink salt and water and you're good to go.
I'm sure there's some nuance here that I don't quite understand. But I will challenge that thought, I will challenge that paradigm if I understand it correctly, and just say, if the paradigm exists, as one that is attempting to use and store energy more efficiently, then that's silly. There's already one that does it much, much better. You just need to train the body to use that fat, continue to use it efficiently at ever higher intensities. And that can happen through just the process of fat of so-called fat adaptation.
Melanie Avalon: I actually found his work because I was googling because he also was very much into certain types of foods. It's like I said, like low PUFA, high fish.
Dr. Benjamin Bikman: Which I totally agree with.
Melanie Avalon: He's actually a huge fan of fruit. He's not a huge fan of vegetables because of gut issues. The reason I found it is because I was googling like, the foods that I was eating, and I was like, “What is this weird combination of foods that I'm eating?” That's how I found his work, but what I was doing for the longest time and I wish back then I had all the tools that I have now, like my CGM and my Lumen, which uses indirect calorimetry, and Biosense and all these different measures because I'm dying to know because for the longest time I was doing a diet where I was doing 24-hour fasting every-- well, it can't be 24 hours because then you wouldn't be eating, but 22-ish hours fasting every day, and eating for two hours, but I was eating super high carb in the form of fruit, super high protein, low-fat. When I would test my blood sugar, it would always be low in the fast. When I would test ketones, it was usually negative. I just wonder like what was I running on? Was I running on glycogen all day and then refilling every--?
Dr. Benjamin Bikman: Glucose, I would say-- that to me is not a healthy diet, Melanie, just for the record. I don't know how you're feeling and I don't want to upset you, if you loved it. You would have to have been running on glucose. In any amount of fructose that was converting to fat and when you need an excess you'd be able to store some fat for later use because the liver is very good at converting fructose into fat. I confess, I'm opposed to that style of eating just because I don't like-- and you're able to do it, you're healthy. I think if we had been talking about overweight diabetic who's focusing on fruit, I consider that not good. I don't think that's a prudent strategy. Also, I can't help but think there's something wrong when the diet is based almost wholly on foods that, in fact, are not essential to humans.
It is a reality, albeit a little maybe indelicate to say or perhaps certainly not diplomatic, there is no such thing as an essential carbohydrate when it comes to humans. We do not have a biological need for literally any type of carbohydrate, none, zero. There are essential fats and there are essential amino acids, there is no such thing as an essential carbohydrate. Now, I'm not declaring war on carbohydrates. That's not my intention, but I do think that ought to in a way form the way we eat, that ought to be part of how we decide what to eat. We certainly can include plants, carbohydrates, for the sake of enjoyment, I think that's very relevant. But fats and proteins what our bodies truly need, they are essential.
My philosophy is focus on those two, and then let the carbohydrates be sprinkled in the diet. Moreover, independent of what we need to eat. I espouse that perspective also because much of my research has concluded that an ideal life is one that is spent not spiking insulin all the time, that is a healthy lean life. Fat and protein have minimal effects, little or no effect on insulin, whereas carbohydrates, of course, have a significant effect on insulin. Altogether, wrapping those ideas up my sort of philosophy on food, or my pillars is control carbohydrates, not to say don't eat them at all, but be smart about them. Prioritize protein filled with fat, and then intermittent fast. I do think there's a lot of power and fasting. Sorry, I went a little off topic. I think a diet a diet that is so wholly based on fruits, I do not think that's ideal.
Melanie Avalon: One quick question about there being no essential carbohydrate. I know it's glucose, it's not carbohydrate.
Dr. Benjamin Bikman: Yeah. Glucose is essential. Sorry, I cut you off, though. That's such a common point of confusion where I did very clearly-- my expression was that dietary carbohydrates are not essential. That is not to be conflated with the idea that glucose isn't essential. No, glucose is absolutely essential. That is why the liver is so good at making it, that ultimate giver, that ultimate generous organ, it makes all the glucose the body needs, and the tissues that need it. For example, red blood cells are 100% dependent on glucose, brain cells are not. I don't think any other cell is actually. I think they're every other cell is a mix of what it can burn. Red blood cells are unique, they have an exclusive dependency on glucose. Thank heavens that the liver makes all we need. I mean that. I'm not saying glucose isn't essential to survival. It is. Thank heavens, the body has a way of making it, which is why it's not essential.
When it comes to those specific fats and those specific amino acids, they are essential because the body cannot make them, and so we must eat them. Glucose is essential, but it's not essential in the diet, because the body is able to make it.
Melanie Avalon: One of the reasons and I'm so allured by fruits is because it seems to have less of an effect on insulin. So, it seems a way to get a higher carb load without the potential issues of all the excess insulin. Like fat generation, just from a hypothetical, like, philosophical perspective. Fat created from carbs, if fat is great and essential, is fat created from carbs, how is that a problem? Because I know most people to do that it's going to be probably in a high insulin inflammatory state, so I can see how that’s a problem. If it's not in that context, is there a problem?
Dr. Benjamin Bikman: It's a great question. No, but I would say that the carbs would never turn into the essential fats, just to clarify, where me saying that there are essential fats in the diet. Those are fats that carbs could never turn into, we have to eat those as fats from fish, for example, or indeed, any animal source literally. Any animal source fats will give those essential fats and essential amino acids incidentally. No, it's not an inherent problem that carbohydrates can be made into fat, not at all. In fact, that appears to be necessary for when we're growing new fat cells, it's that glucose-derived fat or glucose converted to fat. Lipogenesis, that appears to start the lipid accumulation within a smaller fat cell, but the problem only would come if we're putting a burden on the liver through a lot of fructose.
I don't know that you could eat enough fruit to drive that problem in the liver. It would really be a matter of drinking the fruit. Drinking the pure adulterated fructose, that would be problematic. No, there's nothing inherently wrong in carbohydrate making fat. I wouldn't want to say that at all, and so I won't. The type of carbohydrate we eat does actually affect where we store fat. There was a study in humans that had been drink isocaloric drinks of pure glucose or pure fructose, they both gained a certain amount of fat. The glucose drinkers gained it relatively more in the subcutaneous, and the fructose drinkers gained at relatively more in the visceral space, very likely, because it was the liver making all of it when it comes to the fructose-induced fat production.
No, there's nothing inherently bad about carbohydrates being sufficiently ingested to promote fat storage. In fact, evolutionarily, that would have been a good thing. Anything we can get our hands on, let's try to get what we can to store energy for later use and fat would be the optimal way of doing that. It doesn't change. I wouldn't then use that to change my earlier comment. There are essential fats in the diet, but there's still nothing essential about a carbohydrate. Again, I wouldn't want anyone to listen to this and think, “Oh, well, Ben thinks we should all be carnivore.” Not at all. I'm not at all saying that. Not even a little am I saying that.
I'm just saying that to state that, to me, that would be a basis to scrutinize the diet and say, “Why am I getting almost all of my food from the one macronutrient that's not essential? Maybe I should focus more on the essential ones first, and then let this third non-essential macronutrient just fill the gaps,” so to speak.
Melanie Avalon: Yeah, I just want to say thank you so much for engaging in this conversation with me. The reason I'm asking so many questions is because I'm just so fascinated, especially with the whole insulin issue, that there are people and two seemingly completely polar opposite camps, like the super low-carb, carnivore, that whole world for insulin issues. Then on the flip side, we have people like the high carb, low-fat plant base. I've had Cyrus and Robbie, who wrote Mastering Diabetes on the show. And I just so respect you and your work, and your book was amazing. Thank you for listening to my questions.
Dr. Benjamin Bikman: Oh, I love them. Yes, please, this has been a delightful conversation. I would want anyone to know much of my perspective on nutrition is seen through the lens of metabolic disease, like insulin resistance and type 2 diabetes. My perspectives, I never mean for them to seem inflammatory. I base them just completely on human clinical studies, where if you take a type 2 diabetic and put them on a low-carb diet, or a low-fat diet, never once in the human study has the low-fat diet outperformed the low-carb diet. In contrast, there have been dozens of studies where the low-carb diet has outperformed the low-fat diet. I state this very, very deliberately and very cautiously. I wouldn't say it unless I was mentally citing these dozens of studies.
If we're talking about someone who has elevated glucose, to me, it's common sense. Even if we overlooked the data, to say, “Well, if you're having trouble-- if the glucose is accumulating in your blood, maybe I'll put less in your blood for a time and help you clear through the glucose that you have.” Indeed, that's a bit of a cheeky perspective on it, independent of the abundance of clinical data, but if we're looking at someone with type 2 diabetes, the low-carb diet often will outperform the low-fat diet.
Melanie Avalon: That's a huge, huge question I have. Like I said, I had on Cyrus and Robbie, who wrote Mastering Diabetes, and they talk about a high carb low-fat approach. They posit that actually, fat, specifically saturated fat is the mechanism of action for impeding insulin use in the cells. That's actually the cause. And that low carb while it lowers your blood glucose, that it actually is creating insulin resistance that we just don't see because they're not eating glucose.
Dr. Benjamin Bikman: Well, they're totally wrong, frankly. They're absolutely wrong. Well, they're not totally wrong. There is truth to this, but they unfortunately, that perspective, which is very common in the plant-based culture or group to say, “Well, saturated fat will block the insulin receptor.” That is true. That is absolutely true. I've in fact literally done those experiments myself and published actual manuscripts and presented data at scientific meetings on this very specific biochemical process whereby that can happen. I will say conclusively, saturated fat is the cause of insulin resistance. The problem is in what data the person is looking at.
For example, the studies that would come to that conclusion, including my own, that saturated fat is contributing to insulin resistance, and indeed, I bet they would cite a couple of my own studies. They are artificial models. I have indeed published on this, that was largely the work of, in fact, my highest impact factor paper I've ever published was one of those-- detailing one of those mechanisms. However, they're artificial mechanisms, those are artificial models. It's when you are treating cells with saturated fat in the culture, the cell culture medium, or you are infusing saturated fat into the animal or the human's bloodstream directly, those are artificial.
In fact, that was a painful process for me, I would want anyone to know, having contributed to that paradigm, that perspective, that saturated fat is a leading driver of insulin resistance, it required me, I needed to step out of my own hole that I dug, scientifically, and asked myself, “Is this a real model?” The answer is no. What happens then when a person is eating saturated fat, that's the question that should be asked. Remarkably, eating saturated fat does not contribute to circulating saturated fats. This has been shown in some of the work by Volek and Phinney, some of the great low-carb gurus-- they would hate that term, and I do too. Some of the great contributors to what we know with regards to low-carb diets, on the low-carb diet, their low-carb group was eating three or four times more saturated fat than the low-fat group. Remarkably, not only did they have significantly greater improvements in insulin and glucose, but they also had significantly-- they did not have a significant increase in their saturated fats in their blood, and that's because there's nuance that needs to be appreciated. When someone needs saturated fat, that saturated fat does not just spill into the bloodstream, unless it's a short chain, no medium or short-chain fat. Even though those are unsaturated fats, the medium and short-chain fats, they actually stimulate insulin sensitivity, that's quite well established, including the shortest of the shorter-- the saturated fats, acetic acid or vinegar, those improve insulin sensitivity despite being completely saturated.
Nevertheless, in this study, they found no increase in plasma circulating saturated fats, and in contrast, and improvement in insulin sensitivity. Eating saturated fat is not the same as treating cells with saturated fat or infusing it directly into the bloodstream. Those are two, of course, very artificial studies. Once again, so we ask, “Well, what provides-- what dictates the amount of saturated fat in the blood?” The predominant saturated fat in the blood is palmitate. If someone has an increase in palmitate, it's actually because the liver is making it. The liver very readily produces palmitate through a process called lipogenesis. Once again, it comes back to the hormone insulin. Insulin dictates lipogenesis. If insulin is elevated, so you can have someone who's eating zero saturated fat, and yet, they could paradoxically have an increase in saturated fat in their blood, because they're spiking their insulin all the time. Insulin tells the liver to make palmitate, the predominant saturated fat, and then to release that into the triglyceride-rich lipoproteins like VLDL. Saturated fat does cause insulin resistance in artificial models.
In the whole human, when the person has ingested saturated fat assuming that insulin is low, there's zero evidence to suggest that saturated fat, first of all, accumulates in the blood, and second, is contributing to insulin resistance.
Melanie Avalon: To clarify, talking about saturated fat being an issue with messing with insulin and how it interacts with the cells, is that when we eat saturated fat, it does not necessarily pop up in the cell to do that?
Dr. Benjamin Bikman: Yeah, it gets carried on the chylomicron, and then it gets largely taken up by the liver. When a saturated fat is stored or comes to a cell, if it even gets to the cell, often the saturated fat is elongated and desaturated, oddly enough, and that is why even if someone's eating purely saturated fat. If you actually look at the composition of fat in their fat cells, it's almost completely oleic acid. It's 18:1, the monounsaturated fat, because that's how the fat cell stores fat. Oleic acid is the predominant stored fat, regardless of what type of fat they're eating, even saturated. The cells will elongate and desaturate that saturated fat typically, in order to store it as 18:1.
Melanie Avalon: Isn't olive oil really high in oleic acid? Is it benefits?
Dr. Benjamin Bikman: Well, I don't know, actually. That's a good question, because based on what I said, someone could counter and say, “Oh, wait, if 18:1, oleic acid, olive oil, fat is the preferred fat in the body, then I'm not going to eat as much and then I won't store as much.” And, of course, that doesn't happen that way. Interestingly, 18:1, in these same studies that I just mentioned, where we would expose something to pure saturated fat in what is we need to be clear in artificial model, then if we actually co-incubate or co-infused with 18:1. The 18:1 stops the saturated fat from actually becoming ceramides and antagonizing insulin signaling.
What the saturated fats are attempting to do, the 18:1 in the case of insulin resistance undoes or prevents. I did that study very directly, I expose muscle cells to palmitate, and muscle cells with palmitate and oleate in equal amounts. It completely prevented the palmitate from doing anything. I think that there's something important there, and these natural, certainly animal-based fats are tremendously varied source of fat, that we look at beef, and we'll say, “Oh, look at all that terrible saturated fat.” Well, depending on the animal, that fat can almost be as much unsaturated, monounsaturated as it is saturated. So, it's not really fair for people to look at animal meats or animal fats at all, and just assume it's all saturated. There's some beautiful nuance there, and I would say that there's no-- there's zero natural fat. The natural fats I consider to be animal fats and fruit fats that are purely saturated. The most saturated of all, is most certainly, actually coconut oil.
Coconut oil is almost totally saturated, far, far more than any animal source of fat, literally any. It's much, much more totally saturated than any animal source of fat. The actual clinical studies in humans find that if you give people coconut oil, it's better for them, you give animals, an isocaloric diet that has either coconut oil, or soybean oil, and the soybean oil will make them fatter than the coconut oil, even though they're eating the exact same amount of calories. I am not at all a fan. I think it is totally unjustified to throw saturated fat under the bus, most certainly in the context of insulin resistance. There may be other reasons for someone to fear saturated fat if they're very worried about their lipids, and they have familial hypercholesterolemia. I'm not trying to just say saturated fat should get a green light in any instance. Although I think often they should because they're natural fats and their ancestral fats. We've evolved very well on eating them to say that dietary saturated fat is going to cause insulin resistance in a human. I don't believe there's evidence to support that.
Melanie Avalon: One last quick nuanced question. You said something about how the saturated fat in the context of low insulin does not go down that pathway. What about in the context of a mixed diet, high insulin and desaturated fat?
Dr. Benjamin Bikman: No, I totally get what you're saying. Let's say the person who's eating the plain hamburger patty or the patty with the bun. I think that's a relevant question. I cannot say the degree to which that saturated fat is going to change how it's going to be digested and absorbed through the lymph into the chylomicron if insulin is high. I don't know of any evidence to support that idea, but I would say eating saturated fat and making saturated fat because of the spiked insulin from the bun, that's probably not great. Well, for any number of reasons, and saturated fat would be the least of them, frankly. But even still, Melanie, I'm thinking about that. I'm thinking, “Well, what if it was the bun and an equal amount of olive oil by calorie being consumed, pure olive oil?” I don't know. There's just no evidence. I'm not aware of any evidence and I obviously am having a hard time thinking through that. I will say this, that's probably not a great mix. I don't think the bun and the patty should be eating together for any number of reasons, and saturated fat might be one of them.
Melanie Avalon: Well, actually, to that point, because this is the question I've had, I asked them that Cyrus and Robbie. Then you talked about in the book, but you had the opposite answer that they gave. That was, as far as like insulin resistance potential issues, the ordering of fats and carbs because the way I was thinking about it was if you ate the carbs first, they would-- And maybe I think about this too, simplistically, but if you eat the carbs first, I assume they would either get burned or stored as glycogen. Then, if you ate fat-- I guess I might be thinking of it wrong now that you explained how fat doesn't really create that clog up effect. I was thinking there could be a problem if you ate the fat first and it was entering cells and then blocking insulins ability to let carbs in, and then maybe the carbs would not be able to gain entrance. I'm probably thinking about this way too simplistically.
Dr. Benjamin Bikman: Well, I don't know that you are. Fat going into a cell does not make a fat cell, does not make a cell insulin resistant, that needs to be stated very conclusively. Part of this is very well documented in something what's called the Athlete’s Paradox, where some scientists, I think they were UPenn found that people were suggesting-- Well, all this fat storage in the obese muscle is contributing to the insulin resistance, and then paradoxically, they found that athletes had just as much fat stored in their muscle as obese people, endurance-trained athletes, and yet they were exquisitely insulin sensitive. Fat entering into a cell that most certainly does not make the cell insulin resistant.
Now, of course, some fats can, namely ceramides can antagonize the insulin signal. A cell isn't just going to make ceramides willy-nilly, certainly not to a high enough level to become a problem. You need a signal to stimulate the ceramide synthesis. For example, inflammation, or excessively elevated insulin, both of those-- I've actually published papers on both of those exact topics, detailing how that happens. The idea that the fat comes into the cell and blocks the insulin receptor, that just not quite accurate, or it's just overly simplified. You have to have additional signals that come in to play to tell the cell what to do with that fat, to make it into ceramides. Of course, that does mean fat has some role.
The order of eating, I don't know what data they were invoking when they say that it should be carbs first, and then the others. I would say, for the sake of fat mass, it doesn't matter. If you're eating fat and carbs together, you're going to get fat, whether it's the fat first or the carbs first, it doesn't matter. I would say, what I'm speculating, I don't know, the studies have looked at that, that far. But I do know for a fact, because of the studies that I cited in my book, that when you eat fat and protein first, and then it's the carbohydrate at the end, that does yield a significantly different insulin curve and glucose curve from eating the carbohydrates at the beginning. That's why I said it the way I did in the book, put carbs last.
In practice, I don't know how much that really should affect any person's method of eating. This is silly, of course, but someone eating a hamburger, and they said, “Well, I really want that bun. I'm going to eat the patty first, and then I'm going to eat the bun.” In reality, people eat them together. Once again, it's sort of splitting hairs. I do believe one of the plagues of the modern diet is high-fat, high-carb. Those two don't come together in nature. In fact, carbs don't really come with anything in nature, carbohydrates tend to come alone. A fruit is like purely carbohydrate, whereas nature has proteins and fats come together. I understand there are some carbohydrate kind of protein sources, like beans, for example, or nuts, but those kinds of proteins can never-- they truly don't, compared to the amino acid profile or the absorption potential of animal-source protein. I think a diet that is trying to get its protein from plants-- a human diet, is trying to get all its protein from plants is going to be protein deficient.
Frankly, not to mention, well, one, because they won't get the full complement of amino acids that they need. Certainly not from any single plant. Then plants have anti-nutrients in them. Especially if you're looking at a processed plant protein like pea or soy, we know that they become enriched with molecules that directly inhibit protein digestion in the gut, like trypsin inhibitors or phytic acids. Those are genuinely real molecules. Not to mention the heavy metals like lead and arsenic that can come in process plant proteins as well. Nevertheless, in nature, most of the carbohydrates that we eat are pure carbohydrate, and whereas the protein that we eat if we were focusing on protein, it always comes with fat. Once again, I'd say nature is sort of hinting at perhaps how we ought to be building our diet.
Melanie Avalon: One more question about all of this. I've hinted at it a few times, but when people go on low-carb diets, you talked about this, all the studies show that there's so many beneficial changes in insulin sensitivity and blood glucose levels and all of these things. What about the idea of physiological insulin resistance and that go on these low-carb diets that you actually are losing some ability to tolerate carbohydrates?
Also, I can tie in one more little question to speak another question that ties into it as well, but it's the similar concept. It seems that in the context, if you keep this diet, that's low-carb, and you keep insulin levels low, and you keep blood sugar, glucose controlled, it seems to be very beneficial, reversing disease, bringing back health, all these great benefits, but I just wonder, do you have to be on that for life? Are there problems if you fall off of it?
The similar question I have is like, you were talking about LDL, and you talk in your book at length, I learned so much about HDL and the different types of LDL, and everything that's going on there. A lot of people on lower-carb diets will see higher LDL levels, and maybe in the context of that diet, it's helpful and non-inflammatory and protective, and even healing. Then, is it a case where if they have some carbs or change things up that now their body is because of the high LDL going to be in a more precarious state? I know you've been on Paul Saladino on his show, and I've had him on twice. I know he talks a lot right now about his like, really, really high LDL levels, but that in context, it's okay. So, existing in the state.
Dr. Benjamin Bikman: Yeah, these are great questions. First question with regards the physiological insulin resistance. I don't approve of how people use that term. Insulin resistance, I maintain, is defined how I defined it earlier, which is some cells are compromised in their insulin signaling. The second aspect, I believe, must be included in that definition, which is that insulin levels are higher. I appreciate that one person may say, “Well, that's not how I'm defining insulin resistance.” So that might be the problem, where there's just simply not a common vernacular, but I will strongly defend that definition and would do so, in any court of law or court of science.
Physiological insulin resistance is a thing, but I do strongly believe it's invoked incorrectly. The insulin resistance that I study, as a practicing, publishing, presenting scientist, is pathological insulin resistance. So that which of course predominates in our world today, and which is relevant to weight gain in virtually every chronic disease in ways that we've touched on previously. However, not all insulin resistance is bad, and that is the physiological insulin resistance. To my knowledge, the only instances of this are the two Ps, pregnancy and puberty. Those are both times where the body has deliberately altered its insulin signaling, potentially, to just fuel some explosive growth or some selective growth in the body, and to stimulate excess levels of other hormones involved in, say, reproduction.
In both of those instances, puberty and pregnancy, insulin is elevated. Once again, even in this context of physiological insulin resistance, so insulin resistance that is serving a purpose, to either grow the little boy or girl, or for mom to grow a baby, once again, hyperinsulinemia is part of this definition. I'm defending that definition that insulin resistance is a state of hyperinsulinemia. That's part of why having defined that and presented it that way, that's why I resent the term physiological insulin resistance being invoked in the context of a low-carb diet. It's because insulin drops wonderfully. Insulin is not elevated, they have normal or low insulin below normal, it's not deficient insulin, I should be clear to say, That to me, right there immediately tosses out that definition.
When we do these kinds of studies, certainly in an animal model, which is a little problematic, of course, but if they have adapted to a smart ketogenic diet, which is to say one that is not enriched in soybean oil, like most animal studies are, unfortunately. If we give them a load of insulin, they respond to that insulin dramatically, and their glucose levels drop a great deal. In humans, it's a similar phenomenon. There is no evidence, none, to suggest that a human becomes insulin resistant in any way when they have adopted and adapted to a low-carb diet. None. I know of no single manuscript to suggest that they've become insulin resistant, as a result of adapting to that low-carb diet.
What might be some of the truth in people embracing that perspective is that people can become somewhat glucose-intolerant, with long term adherence to a low-carb diet. I refer to that, to my knowledge, I'm the only one who refers to it, so maybe I've made this up, or others are equally clever if I can pat myself on the back. It's a reverse metabolic inflexibility. Very briefly, in insulin resistance, what abounds, and because insulin resistance is so common, this is so common, people are metabolically inflexible in favor of glucose. Metabolic flexibility, you know, and I'm sure your listeners know, so I'll be very brief. It's just this phenomenon whereby a person can shift between glucose burning after they've eaten, in a few hours after they've eaten when they've entered a so-called fasted state, now they shift to fat-burning, and they can, they can shift between these two fuels, operating like a clean hybrid metabolic engine.
Unfortunately, with type 2 diabetes, or insulin resistance, pre-diabetes, a person is stuck in glucose burning mode. And that's a result of the chronically elevated insulin because insulin dictates fuel use. Something I mentioned at the beginning of the discussion. If insulin is elevated, the body is predominantly burning glucose. Although, of course, unfortunately, not too well, and that's partly why we see the glucose climbing and the individual. In this case, that is metabolic inflexibility, in favor of the glucose. The person eats their glucose burning mode, they fast, so hours later, they're still in glucose burning mode. They haven't shifted to fat burning. In contrast to this and stark contrast, someone who has been adhering to a low-carb diet for a sufficiently long time to adapt, however long that would be, and there's no definite time point there. Let's say it's been long enough to adapt. They are, if you will, stuck in fat-burning mode, that is most certainly and I would vigorously defend it that is not as pathological, as being stuck in glucose burning mode, if for no other reason, then the glucose burning metabolic inflexibility is typified by chronically elevated insulin, which drives a host of pathologies. In contrast, being stuck, if you will, and fat burning, being metabolically inflexible in that direction, would be typified as low insulin. There's not a single pathology that would arise because of normal or low insulin.
Nevertheless, there's something to be said for that. The person is metabolically inflexible in favor of fat. If they load their system with glucose, it will take them longer to clear that glucose than it would have, perhaps, before they started the low-carb diet. That there I think, is part of why people say physiological insulin resistance, that is a misnomer. It is an inaccurate term, and I do think people should stop using it. They should say either a reverse metabolic inflexibility if they want to quote Dr. Bikman, or they could say they are glucose intolerant. That is not the same. that is not the same as insulin resistance, because if you give them a load of insulin, they will have very low levels of glucose very, very quickly.
The man I mentioned earlier, George Cahill, has done some of those experiments in people that were fasted, and naturally fat-adapted. Give them insulin, and their glucose plummets, that right there refutes the idea of insulin resistance in any way, shape, or form. Low-carb adaptation or fat-adaptation is not insulin resistance at all. I would say it does serve a purpose. It is a physiological phenomenon, but they have become glucose intolerant, it's essentially the body's way of saying, “I'm not eating glucose. I have fat and fat is what I'm fueling on. So, I've turned off the glucose burning mechanisms.” And it simply takes a couple days to turn it back on. If someone needed to go in and pass a glucose tolerance test in a clinical setting, and they've been long-term adhering to a low-carb diet, and I would say, “You know what, you should probably spike in the carbs over the next few days to prepare, and then you'll go into that testing, you'll pass it perfectly fine.” They very, very likely would.
Melanie, having said all of that, I would also want someone to say that, as much as I am an advocate of a low-carb diet for someone who has concerns with regards to metabolic health, I'm also quite practical, and in so, I don't believe, unless a person has a genuine clinical reason, like say epilepsy where they have to stay in ketosis to control their seizures. I don't think there's a reason someone has to be extremely strict. I am very favorable with regards to fruits and vegetables. Certainly, in my diet, and even the people I talk to, so my kind of my pillars that I outlined earlier, which starts with control carbohydrates, when someone asks me to define that one step further, you're not asking, but I'm going to tell you anyway. I say actually focus on fruits and vegetables. In general, if you're focusing on eating, fruits, and vegetables and you're being careful with the starchy grains, and certainly the sugary junk food, that is a great strategy. Then just eat those fruits and vegetables, don't drink them.
I think if someone is doing that, and even though they're shifting more of their focus to protein and fat, but they're eating fruits and vegetables, which again, I'm totally in favor of, I don't know that they would ever develop even that degree of glucose intolerance, or that reverse metabolic inflexibility that I mentioned. That's why I'm an advocate of that.
In the end, just realizing the nature of the world that we live in, if someone were just simply going to say, “I'm never going to eat carbohydrates ever again.” I'd say, “Well, then you're done. Any kind of glucose intolerance you develop, it's irrelevant. It won't matter.” If they're living in a world where they will, from time to time be eating carbohydrates, like I have my little kids, and we have some little party or something, or even more often, one of my daughters wants to make dinner, and it's a starchy kind of pasta type dinner, I'm absolutely going to eat that. There's no question I'm going to eat what my darling little daughter made for me, or anything anyone makes in my family. I think that if we acknowledge the kind of the lay of the land, the reality of the world, which is that carbohydrates are going to be around and you're probably going to eat them, well, then that might be a reason for someone to always have some of them in their diet. If a person is a type 2 diabetic, then I strongly maintain, they would simply have to be more careful and more strict than someone who's doing it maybe-- like, in my case, someone who's doing it to just stay lean and keep disease at bay.
Melanie Avalon: Really quick question to that with the fruits and vegetables. You talked about the difference between the glycemic index and glycemic load. That actually was a mindful moment for me because when I was eating the really, really high fruit, I was eating a ton of pineapple. It's actually a seven on glycemic load. I was like, “Oh, that is so interesting.”
Dr. Benjamin Bikman: Pineapple is so yummy. It's so delicious.
Melanie Avalon: It breaks down protein really well, too. I was eating basically, like tons of meat and pineapple.
Dr. Benjamin Bikman: Even then, Melanie, if I were talking to a type 2 diabetic, and then that would be my next level, that I would have started with control carbohydrates and say, “What do you mean?” I would say, “Well, focus on fruits and vegetables.” Then I look at the type 2 diabetic and say, “Well, actually for you, focus on the least of the sugary fruits and vegetables. Be careful with pineapples and mangoes, for example, and the starchiest of the vegetables, like potatoes, for example. Then anything else, generally you're going to be fine with.” Citrus fruits, I'm very okay with personally. Any vegetable that grows above the ground, even with the strictest of type 2 diabetics, I would say, you could eat that liberally. That's my next level, depending on the person and their concern and their worry with type 2 diabetes.
Melanie Avalon: Okay, gotcha. Well, I have so many more questions, but I want to be really respectful of your time. One last thing, maybe we can dive in really deep. Do you wear a CGM?
Dr. Benjamin Bikman: I sure do. Yeah, in fact, I bet you've probably worked with Levels to get yours. Is that right?
Melanie Avalon: Yeah.
Dr. Benjamin Bikman: Yeah, I have one on right now.
Melanie Avalon: Mine just expired yesterday, so I have to put on the new one. It has been the most eye-opening thing ever. For listeners, the CGM, it monitors your glucose constantly. You can see how you react to foods, to fasting to everything. Like I said, my fasting blood sugars were fine, they were in the 90s, but I wanted them lower. I started taking berberine, and it's been shocking what it does to my blood glucose.
Dr. Benjamin Bikman: It brought it down?
Melanie Avalon: Yes, it's crazy. Now they're stable in the 70s every day.
Dr. Benjamin Bikman: There are these molecules, like berberine, and even cinnamon and an apple cider vinegar, that can help bring it down. I'm very warm minded on those kinds of supplements if someone's trying to control their glucose. I'm also quick to say that if I were talking to a type 2 diabetic, who continues to eat a very high sugar, high starch diet, I would say all the berberine, all the cinnamon in the world isn't going to help you if you don't have your macros managed. My perspective on those supplements is, mind your macros. Then, if you need a little boost, if you need a little more nudge, then absolutely things like berberine and some others, a handful of others can absolutely help make up that last little bit of difference.
Melanie Avalon: Yeah, it was really incredible. I think I got a little bit too excited, and I made myself a little bit hypoglycemic a few times. I was like, “I got to figure out how to--” [laughs] I tend to go crazy. Listeners, you have got to get Why We Get Sick. I mean, this has been a two-hour conversation and I didn't even get to like half of the things I wanted to ask you. There's so much in this book. Friends, get the book, it will open your eyes to so many things. He talks about so many things that we didn't talk about, all of these different health conditions and how insulin relates to them. The diet, the exercise protocols, which we touched on briefly in this episode, but dives in deeper, the science, how stress affects insulin. I mean, so many things. I cannot thank you enough for this book. I feel like I've been waiting for this book for years. On my other show, like I said, the Intermittent Fasting podcast, Gin and I talk about insulin all the time. It's just so nice to see it finally, being made more public with things like your work, so I really cannot thank you enough.
Dr. Benjamin Bikman: Oh, my pleasure, Melanie. Thanks again. I'm so delighted you reached out. This has been time well spent. I hope that your listeners feel gratified and educated.
Melanie Avalon: I promise this last question. It's literally the last question I ask every guest. It's just because I realized how important mindset is, so what is something that you're grateful for?
Dr. Benjamin Bikman: Oh, thank you for asking. I am now more than ever, I am so grateful for my family. Sometimes I try to find ways to work this into conversations. As much as it seems, someone listening to this would just think, “Boy, Ben is a scientist.” Sure, I am, but that's just a means to an end. That's a hobby. I am a husband, first. I'm a father, second, but don't tell my kids that. My loyalty is to my wife first, but my kids are right there, too. My family. I'm so grateful for my family, that might seem kind of trite or cliche. When the world gets crazy, I think it helps us look more inside. For me, that's looking at my home, and really asking what I'm doing to help my family, to protect my family, to raise my family. There's a tremendous responsibility. It's overwhelming often, but that is, at the end of every day what I'm most grateful for.
Melanie Avalon: I love that so much. Well, thank you. Like I said, I'm so grateful. Listeners, get the book. Are there any other links you want to throw out there?
Dr. Benjamin Bikman: Yeah. Well, thanks again. By all means, go buy the book, if this conversation was stimulating, you'll have a lot more material, that you'll find engaging in Why We Get Sick. Also, I'm involved with an education platform called Insulin IQ, which hopefully will be making a ton of coaching aspect to that, and then gethlth.com, H-L-T-H. That's how health is spelled, in this case, gethlth.com, is a venture I've started with a couple of my brothers just to make a better low-carb shake. Then, I'm fairly active on social media, mostly Instagram, which I've just found more and more. It's funny, I started on Twitter, and it's just increasingly hostile. I don't like Twitter as much. The Instagram crowd is just so much nicer. Anyway, on Instagram, @BenBikmanPhD. Bikman is just B-I-K-M-A-N, no C. @BenBikmanPhD.
Melanie Avalon: Awesome. For listeners, I will put links to all of that in the show notes. Again, the show notes will be at melanieavalon.com/insulin. Thank you so much. This was so incredible. I'm so happy right now, and hopefully, we can talk again in the future because this was amazing.
Dr. Benjamin Bikman: I would love it. I had a great time. Melanie, thanks so much.
Melanie Avalon: Thanks, Ben. Bye.